Barrett’s Esophagus
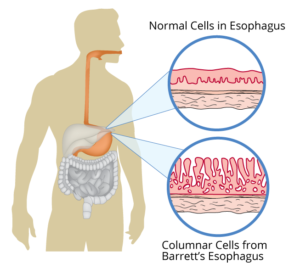
Barrett’s esophagus refers to a change in the esophagus lining from tissue resembling normal mouth lining to something that looks more like stomach lining with specialized mucus secreting cells. Chronic acid injury is the favored theory regarding the occurrence of Barrett’s esophagus.
Symptoms
Barrett’s esophagus produces no particular symptoms. Most people seek help and are diagnosed because of symptoms of GERD, including heartburn, regurgitation, a persistent cough or difficulty swallowing.
Risk
People with GERD do not necessarily develop Barrett’s esophagus. Conversely, people who develop Barrett’s esophagus do not always experience GERD symptoms. Still, Barrett’s esophagus is most common in people who have experienced GERD symptoms over a longer period of time. Other factors that influence risk for Barrett’s esophagus include:
- Gender—men are twice as likely as women to contract Barrett’s esophagus
- Age—More common in people over fifty
- Race—more common in Caucasians
- Lifestyle—more common in overweight individuals
Smokers are more likely than non-smokers to have Barrett’s esophagus.
Those with Barrett’s esophagus have a small but increased risk of developing cancer of the esophagus called esophageal adenocarcinoma.
Diagnosis
Your doctor can diagnose Barrett’s esophagus by:
- Taking a medical history
- Performing a physical exam
- Performing diagnostic tests, such as an upper endoscopy
Treatment
In patients with Barrett’s esophagus it is important to control reflux symptoms in order to stop the damage to the esophageal lining.
LIFESTYLE MODIFICATION Perhaps the most important part of any anti-reflux plan involves lifestyle modification.
Alter Dietary habits
- Avoid overeating
- Avoid eating 2 to 3 hours before bedtime
- Avoid eating foods that may trigger symptoms. Follow the dietary guidelines in the diet section below.
- Eat slowly
- Avoid hard candy and chewing gum which increases swallowed air and consequently may increase reflux
Lose weight if needed, although thin persons may have significant reflux
Avoid tight clothing
Quit smoking or using tobacco products, and avoid second hand smoke
Elevate the head of the bed to decrease stomach acid from flowing up into the esophagus.
DIET Patients who are overweight or obese should talk with their doctor or dietitian about dietary changes that can help with weight loss and decrease GERD symptoms.
Unfortunately, there is no “one-size-fits-all” diet to reduce reflux symptoms, and foods that bother one patient may not bother another. However, a list of the most common foods that trigger acid reflux are found below.
- Fatty, spicy or fried foods, red meats
- Coffee (with or without caffeine) and caffeinated beverages
- Alcoholic beverages
- Carbonated beverages
- Garlic, onions and peppers
- Citrus fruits and juices
- Tomatoes
- Chocolate and peppermint
- Fast foods
- Whole milk, cream and creamy soups
Medication
Since reducing reflux is an important goal in treating Barrett’s esophagus, you should be sure to discuss your medical regimen with your doctor to identify medications that may be contributing to the reflux problem. Some medications weaken the normal esophagus barrier while others contribute to GERD by slowing stomach emptying. We strongly discourage patients from stopping medications; even those that might cause reflux, without discussing the potential hazards with their physician.
In the long run, medical therapy may not be enough to overcome poor dietary habits and lifestyle choices. However, doctors may suggest or prescribe medicine to manage reflux symptoms and reduce the effects of acid in the esophagus.
Proton Pump Inhibitors are typically prescribed for Barrett’s Esophagus.
PPI’s are similar to H2 blockers in that they lower the amount of acid the stomach makes, but are more potent and can work up to 24 hours. It is important to take this class of medicine regularly to maximize it’s effectiveness. PPIs can heal the lining in some people who have significant esophageal damage due to GERD.
Side effects from PPIs may include cramps, diarrhea, and occasionally headaches. Proton pump inhibitors are one of the most widely prescribed medication classes. Our practice continues to monitor the concerns about the risks of these medications. Concerns have been heightened by studies showing a relationship between this class of medications to the following conditions:
- Dementia
- Chronic kidney disease
- Bone fractures
- Increased risk of gut infections like Clostridium Dificile colitis
- Low magnesium levels
A causal relationship has not been demonstrated in the above conditions and the use of PPIs.
We agree with the positions taken by the American College of Gastroenterology. First, this class of medications has clear benefits to many patients with esophagitis, ulcer disease, and bleeding related to acid related disorders. Secondly, many people currently taking PPIs have been started on the medication and never stopped when it was appropriate to come off the medication. Third, many people use these medications to allow them to avoid the important lifestyle changes which would reduce or eliminate their symptoms.
We strongly advocate taking these medications at the lowest effective dose for the shortest period necessary to avoid serious gastrointestinal problems. Our practice encourages patients to implement lifestyle changes that allow changing to lower potency acid inhibitors, like H2 blockers, or occasional antacid use when possible. The decision to continue this class of medications should be made after careful assessment of the risks and benefits of continued therapy.
PPIs that doctors may prescribe are:
- Protonix (pantoprazole)
- Prevacid (lansoprazole)
- Nexium (esomeprazole)
- Prilosec, Zegerid (omeprazole)
- AcipHex (rabeprazole)
- Dexilant (dexlansoprazole)
Procedures
Long term reflux or reflux that does not respond to usual therapy may lead your physician to recommend an upper endoscopy. If Barrett’s esophagus is identified further exams may be required based on determination of the level of tissue abnormality.
Surgical Interventions
If Barrett’s Esophagus symptoms don’t improve with dietary and lifestyle changes or medications, sometimes a doctor may recommend surgery. Fundoplication is the most common surgery for Barrett’s Esophagus and GERD, usually leading to long-term control for reflux. A surgeon uses a laparoscope to sew the top of the patient’s stomach around their esophagus in order to provide support to the valve between the esophagus and the stomach, reducing reflux. The surgery is conducted under general anesthesia and patients are usually able to leave the hospital in 1 to 3 days.
Do you have Barrett’s Esophagus or have symptoms that make you wonder if you do? Our office can help. Call (706) 868-0104 for more information.
The content on our website is for informational purposes only, and is not intended to diagnose or treat any medical conditions. Always seek the advice of your physician with any questions you may have regarding your health.